
The isolation of the pandemic can cause some older Americans to feel depressed—but doctors can help.
Nearly Two-Thirds Of Seniors Who Feel Depressed Won’t Seek Treatment
(NAPSI)—Many older Americans say they feel depressed—yet the majority of them are not planning to get help, according to a new national survey—though it could make a tremendous difference in their health and well-being.
With the onset of colder weather, fewer daylight hours, and the effect of the pandemic on holiday celebrations and traditions, more seniors than ever could be struggling with depression.
The GeneSight Mental Health Monitor reported that about two-thirds of adults 65 and older who are concerned they may be suffering from depression say they won’t seek treatment. That’s compared to fewer than half of adults over age 18. In addition, three in 10 of these older adults think “they can just snap out of it.”
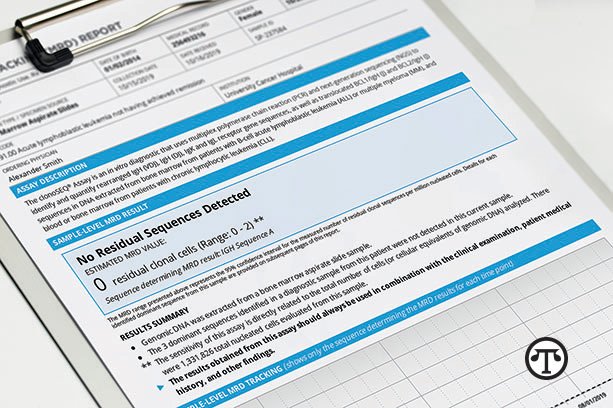
“The ‘pull yourself up by your bootstraps’ mindset and reluctance to talk about mental health may be preventing seniors from getting the help they need,” said Dr. Mark Pollack, chief medical officer of Myriad Neuroscience, makers of the GeneSight test, a genetic measure that identifies potential gene-drug interactions for depression medication. “People seek treatment for conditions like heart disease, high blood pressure or diabetes. Depression is no different. It is an illness that can and should be treated.”
One GeneSight patient, Carmala Walgren, a 74-year-old resident of New York, agrees that depression should be treated regardless of age.
“There is such a stigma about depression among people my age,” said Walgren. “It is worth it to find treatment that helps you.”
Canceling Holiday Celebrations and The Effect on Mental Health
The pandemic is taking a toll on the mental health of older Americans. Nearly one in four people over age 65 said that the news about the pandemic has left them “feeling consumed with sadness.” For those seniors who think they might have depression, the number climbs to nearly 4 in 10. Concerns about COVID are also why more than one in three seniors worried about being depressed say they are “somewhat” or “very likely” to cancel holiday celebrations such as Thanksgiving.
Even as some consider canceling holiday festivities, isolation from friends and family remains a concern. Just under half of these seniors say they feel “isolated and disconnected from family,” compared with 28% of all respondents over age 65, and 24% of respondents over age 18.
Connecting Can Help with Depression
Parikshit Deshmukh, M.D., CEO and medical director at Balanced Wellbeing, LLC, specializes in geriatric psychiatry. According to Dr. Deshmukh, families should make plans to connect virtually if they don’t feel comfortable about getting together in person. Further, caregivers should be vigilant in looking for the signs of depression in their older loved ones.
“It’s more important than ever to let each other know we care and that we are not alone—even if it feels that way,” said Dr. Deshmukh. “Video calls might not be for everyone. Yet, if that’s the only way to stay in touch, we need to do it.”
And Dr. Deshmukh reminds seniors to talk to their doctors. “If your clinician recommends treatment, ask about the GeneSight test. The results can help them make decisions about medications to treat your depression.”
That’s just what Carmala Walgren’s doctor did. “The results I got from this personalized genetic test helped my doctor and me to finally find the medication that worked for my depression.
He told me that because I was covered by Medicare, there would be no cost for me to take the test.
“The GeneSight test made such a difference in my life,” added Walgren. “I don’t know where I would be without it, especially now.”
Learn More
For further information on older adults and depression, visit www.genesight.com/olderadult.
 (NAPSI)—Heart disease is a leading cause of death for all Americans, but the death rate is higher for African American men and African American women of all ages than for whites.
(NAPSI)—Heart disease is a leading cause of death for all Americans, but the death rate is higher for African American men and African American women of all ages than for whites.

 (NAPSI)—People are increasingly concerned about dirt and germs these pandemic days, but many are neglecting an unseen area where airborne contaminants can lurk: the air ducts.
(NAPSI)—People are increasingly concerned about dirt and germs these pandemic days, but many are neglecting an unseen area where airborne contaminants can lurk: the air ducts.

 Being aware of food portion size, the kinds of foods and beverages you consume, and how often you have them may be a step to help you make healthier food choices.
Being aware of food portion size, the kinds of foods and beverages you consume, and how often you have them may be a step to help you make healthier food choices.

