FOR YOUR HEALTH: Understanding COPD
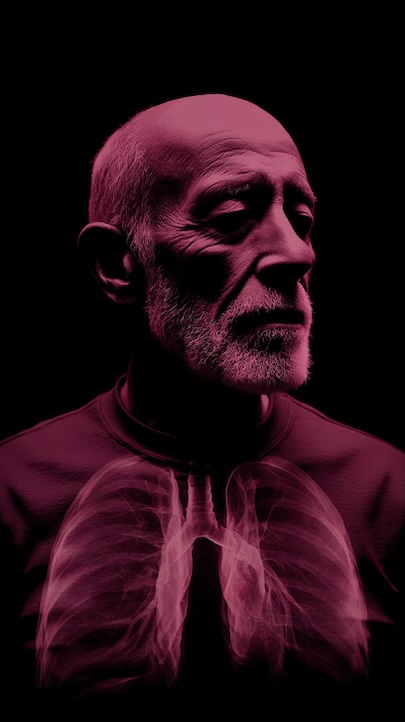 COPD stands for chronic obstructive pulmonary disease, a term used to describe chronic lung diseases, including emphysema and chronic bronchitis. Often, COPD is caused by inhaling pollutants, which includes tobacco smoking and second-hand smoke, but other causes of COPD can be fumes, chemicals and dust found in work environments, and genetics.
COPD stands for chronic obstructive pulmonary disease, a term used to describe chronic lung diseases, including emphysema and chronic bronchitis. Often, COPD is caused by inhaling pollutants, which includes tobacco smoking and second-hand smoke, but other causes of COPD can be fumes, chemicals and dust found in work environments, and genetics.
Two of the most common conditions of COPD include chronic bronchitis and emphysema.
Chronic bronchitis
Chronic bronchitis is a condition where your airways are inflamed. This causes mucus to build up, which can lead to symptoms including:
Frequent coughing or cough that produces a lot of mucus.
Wheezing
- A whistling or squeaky sound when you breathe.
- Shortness of breath, especially with physical activity.
- Tightness in your chest.
Emphysema
In emphysema, the walls between many of the air sacs in the lungs are damaged, causing the air sacs to lose their shape. The damage can also destroy the walls of the air sacs, leading to fewer and larger air sacs instead of many tiny ones. This makes it difficult to breathe.
Symptoms of COPD
Often, people may not recognize the symptoms of COPD until the disease has progressed. COPD can decrease the flow of air going in and out of your lungs, making it hard for you to breathe. Symptoms can vary from person to person, but these are the most common:
Increased shortness of breath/breathlessness. Frequent coughing (with and without mucus), wheezing, tightness in the chest. Unusual tiredness. COPD affects many people – chronic lower respiratory diseases, including COPD, are a leading cause of death in the United States.
If you think you are experiencing any of these COPD symptoms, discuss them with your doctor.
COPD causes and risk factors can vary from person to person, but can include: Smoking, exposure to air pollution, breathing secondhand smoke, working with chemicals, dust, and fumes, a genetic condition called alpha-1 antitrypsin deficiency, and a history of childhood respiratory infections.
The 4 Stages of COPD
A COPD diagnosis and assessments by your doctor can also help identify how far your COPD has progressed and what grade/severity you are. How fast COPD progresses can vary from person to person.
COPD can be classified into 1 of 4 grades based on your ability to breathe. This is determined by specific lung function tests.
Each grade is determined by a calculation taking into account the results of two breathing tests (spirometry), as well as other factors, which include your age, sex, and ethnicity.
The higher the grade (grade 4 being the highest), the more advanced your COPD is.
Grade 1
Severity of airflow obstruction: ≥80 percent of normal percent predicted FEV1.
Mild: Commonly, in this stage, COPD causes mild symptoms, and some patients have shortness of breath.
Grade 2
Severity of airflow obstruction: 50 to 79 percent of normal percent predicted FEV1.
Moderate: Many may seek help for COPD symptoms like shortness of breath.
Grade 3
Severity of airflow obstruction: 30 to 49 percent of normal percent predicted FEV1.
Severe: Typically, in this stage, COPD symptoms worsen and flare-ups may be more frequent.
Grade 4
Severity of airflow obstruction: <30 percent of normal percent predicted FEV1.
Very severe: This is known as the most severe stage of COPD.

 Dietitian answers 5 key questions
Dietitian answers 5 key questions




 by Dr. Greg Carnevale,
by Dr. Greg Carnevale,
