I’M JUST CURIOUS: Yummy pickle juice
 by Debbie Walker
by Debbie Walker
Do you have any idea how many uses there are for pickle juice? I didn’t have a clue. I am passing on more information from my Farmer’s Almanac Newsletter from 7/4/18 (https://farmersalmanac.com/uses-for-pickle-juice-28005). If you enjoy this stuff you really should join if you haven’t already, obviously I am a fan!!
I was surprised to find out pickle juice makes a natural sports drink – you can swig it or make popsicles. I was not real surprised to read the pickle juice is also an excellent way to season your potato salad, just add to your taste.
Other recipe helpers might be to add the pickle juice to flavor your boiled eggs; put juice in the water of your steamer for veggies; boost the flavor in corned beef and cabbage (add a splash to tenderize the meat). Then you could use pickle juice in place of the vinegar to make marinades and salad dressings. You could also use pickle juice and olive oil for a salad dressing, etc, etc.
You may also see the value of it in tomato juice, V8 juice or in your Bloody Mary. One thing I am finding more and more is to make ice cubes out of such and add it that way… Oh and if you are suffering from a hangover you just swig some to hydrate and restore your electrolyte level.
I maybe need to carry some around with me in a bottle. It also mentioned taking a swig to relieve muscle cramps and restless leg problems. Take a swig of the juice for a cure for hiccups or as a heartburn remedy. How about using it for a cough medicine, you got it, you just need a swig. Seems it helps with just a swig for losing your voice or for sore throat. Now for constipation it takes a whole glass of THE juice. Hey, whatever works! Another one I never heard of is to quench appetites, so if you are in my house and see all these dry pickles in the jars you will know what happened. It wasn’t from all the cooking I (don’t) do it was from my using a “new sports drink!”
Fourth of July is long since over, just think of all those jars of juice you dumped down the sink and the new uses you have for them! That’s okay, there are more cookouts to come and of course you can’t forget Memorial Day cookouts.
I would like to take this space to thank all of you with your notes of kindness in the month of July when Mom died. We decided we really can’t be sad because she passed so quickly, no lingering on for her. We are all grateful for that.
I’m just curious if you have ever tried any of these remedies and recipes. Contact me at dwdaffy@yahoo.com and of course Thank You for reading.





 How they can benefit each other
How they can benefit each other

 Next, we’ll look at birds. Poultry manure is strong stuff; when it’s time to shovel out the chicken coop, I try to make sure it’s mixed with bedding as I incorporate it into the soil, waiting a couple of weeks until planting. Alternatively, the careful use of a movable pen or “chicken tractor” moves the birds to a spot where the birds scratch around, eat weeds and seeds, and contribute their “deposits” to nourish the soil. For added nutrition in the birds’ diet, we could move them to a plot where we grew treats for them like greens, pumpkins, grains, and sunflowers.
Next, we’ll look at birds. Poultry manure is strong stuff; when it’s time to shovel out the chicken coop, I try to make sure it’s mixed with bedding as I incorporate it into the soil, waiting a couple of weeks until planting. Alternatively, the careful use of a movable pen or “chicken tractor” moves the birds to a spot where the birds scratch around, eat weeds and seeds, and contribute their “deposits” to nourish the soil. For added nutrition in the birds’ diet, we could move them to a plot where we grew treats for them like greens, pumpkins, grains, and sunflowers.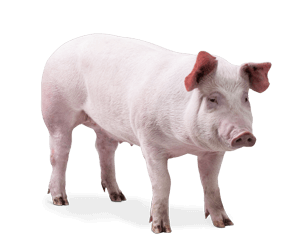
 What about goats? Yes, their manure has been responsible for earning a few blue ribbons. Yes, they are good at mowing the lawn in areas that the lawn mower refuses to go. Yes, they eat all those veggies that didn’t quite make the cut. Yes, yes, yes! But my eyes glaze over when I think of the trouble they’ve made throughout the years whenever they’ve escaped their assigned side of the yard, gone to places they weren’t welcome, crashed my garden parties, gnawing on every fruit tree and seedling in sight. I get it why people want goat milk, meat, and manure — I totally do!
What about goats? Yes, their manure has been responsible for earning a few blue ribbons. Yes, they are good at mowing the lawn in areas that the lawn mower refuses to go. Yes, they eat all those veggies that didn’t quite make the cut. Yes, yes, yes! But my eyes glaze over when I think of the trouble they’ve made throughout the years whenever they’ve escaped their assigned side of the yard, gone to places they weren’t welcome, crashed my garden parties, gnawing on every fruit tree and seedling in sight. I get it why people want goat milk, meat, and manure — I totally do! (NAPSI)—Every day, it’s estimated, 10,000 Americans turn 65 years old. Some of these people, unfortunately, have misconceptions that can jeopardize their health. Major health myths and misconceptions regarding senior health include:
(NAPSI)—Every day, it’s estimated, 10,000 Americans turn 65 years old. Some of these people, unfortunately, have misconceptions that can jeopardize their health. Major health myths and misconceptions regarding senior health include: If I feel fine, I am fine. Chronic infections can last so long that the way they feel becomes the “new normal,” when it shouldn’t be.
If I feel fine, I am fine. Chronic infections can last so long that the way they feel becomes the “new normal,” when it shouldn’t be.